Now That You Started Treatment, What Else Can You Do to Prevent Decline?
Empowering Steps Beyond Treatment: Safeguarding Against Decline
What starts with a commitment to the medical treatment of hearing loss and tinnitus leads to a promise to take best care of yourself by following a holistic and comprehensive treatment plan. Our simple motto that hearing care is health care means it is important that we think beyond the ears and assure you live your best, healthiest, life. We remain steadfastly committed to helping each patient understand how (in addition to treating their hearing loss) they can actively age, remain confident and stay fiercely independent.
Like treating all major medical conditions, the initial prescription (be it a pill to reduce your cholesterol, a round of radiation, an injection to control A1C levels, etc.) must be combined with a healthy lifestyle. The body has an incredible ability to provide relief and heal itself—but only when given the right resources.
We commit to a holistic approach to treating sound, mind, and body. We not only help you hear your best, but we can also help you live your best life as you age and prevent decline. From the technology we use to help you hear your best every day and keep you mentally sharp, we can also help you to increase overall health by discussing diet, supplements, and exercise.
What you hear matters.
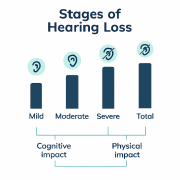
Your brain is always on. Your ears are always on too. This means your brain is constantly stimulated by the vast neural network from your ears. Until it is not. Then what happens?
There is a general belief that activities which stimulate the mind, i.e., hearing, can help to slow cognitive decline. Data tells us that treating hearing loss may even slow the progression of dementia.
What starts out as subtle cognitive changes that are seemingly associated with aging goes on to affect an older adult’s day- to-day function. As we age, there are certain expected cognitive declines that we will all experience. However, with increased risk of cognitive decline and dementia associated with hearing loss, it is important to know the differences of ‘normal aging’, MCI (mild cognitive impairment) and dementia.
Early stages of significant cognitive decline (first seen in MCI) include problems with memory, language, thinking, judgement, and visual perception. Fortunately, most people are still ‘with it’ enough to notice these issues and can seek early intervention. Family and close friends may also notice a change. But these changes often are not severe enough to significantly interfere with daily life.
Common signs and symptoms of cognitive decline include:
- Memory loss such as forgetting names, places, or recent events.
- Problems with organizing or planning—struggling with multitasking.
- Difficulty with recognizing faces.
- Difficulty finding words—often losing vocabulary.
- Misplacing items.
- Problems calculating a tip or paying bills.
- Slower recall which could either be visual or verbal.
MCI along with hearing loss can increase your risk of later developing dementia caused by Alzheimer’s or other neurological conditions, which is why addressing risk factors early such as the medical treatment of hearing loss is critical to preventing dementia.
The proper medical treatment of hearing loss and tinnitus is designed to provide auditory feedback and cognitive stimulation that your brain needs.
What you feed your body matters.
Much like an expensive car, your brain functions best when it gets only premium fuel. Eating high-quality foods that contain lots of vitamins, minerals, and antioxidants nourishes the brain and protects it from oxidative stress—the “waste” (free radicals) produced when the body uses oxygen—which can damage cells.
Diet
Unfortunately, just like an expensive car, your brain can be damaged if you ingest anything other than premium fuel. If substances from “low premium” fuel (such as what you get from processed or refined foods) get to the brain, it has little ability to get rid of them. Diets high in refined sugars, for example, are harmful to the brain. In addition to worsening your body’s regulation of insulin, they also promote inflammation and oxidative stress. Multiple studies have found a correlation between a diet high in refined sugars and impaired brain function.
Just as there is no magic pill to prevent cognitive decline, no single almighty brain food or supplement can ensure a sharp brain as you age. Nutritionists emphasize that the most important strategy is to follow a healthy dietary pattern that includes a lot of fruits, vegetables, legumes, and whole grains.
With that said, certain foods in this overall scheme are particularly rich in healthful components like omega-3 fatty acids, B vitamins, and antioxidants, which are known to support brain health and often referred to as ‘brain foods’. Incorporating many of these foods into a healthy diet on a regular basis can improve the health of your brain, which could translate into better mental function.
Research shows that the best brain foods are the same ones that protect your heart and blood vessels, including the following:
- Green, leafy vegetables. Leafy greens such as kale, spinach, collards, and broccoli are rich in brain-healthy nutrients like vitamin K, lutein, folate, and beta carotene. Research suggests these plant-based foods may help slow cognitive decline.
- Fatty fish. Fatty fish are abundant sources of omega-3 fatty acids, healthy unsaturated fats that have been linked to lower blood levels of beta-amyloid—the protein that forms damaging clumps in the brains of people with Alzheimer’s disease. Eating fish 1-2 times a week can be healthy for your brain (but be sure to choose varieties that are low in mercury, such as salmon, cod, canned light tuna, and pollack). If you are not a fan of fish, ask your doctor about taking an omega-3 supplement, or choose terrestrial omega-3 sources such as flaxseeds, avocados, and walnuts.
- Berries. Flavonoids, the natural plant pigments that give berries their brilliant hues, also help improve memory, research shows. In a 2012 study published in Annals of Neurology, researchers at Harvard’s Brigham and Women’s Hospital found that women who consumed two or more servings of strawberries and blueberries each week delayed memory decline by up to two-and-a-half years.
- Tea and coffee. The caffeine in your morning cup of coffee or tea might offer more than just a short-term boost! In a 2014 study published in The Journal of Nutrition, participants with higher caffeine consumption scored better on tests of mental function. Caffeine might also help solidify new memories, according to further research. Investigators at Johns Hopkins University asked participants to study a series of images and then take either a placebo or a 200-milligram caffeine tablet. More members of the caffeine group were able to correctly identify the images on the following day.
- Walnuts. Nuts are excellent sources of protein and healthy fats, and one type of nut might also improve memory. A 2015 study from UCLA linked higher walnut consumption to improved cognitive test scores. Walnuts are high in a type of omega-3 fatty acid called alpha-linolenic acid (ALA), which helps lower blood pressure and protects arteries. That’s good for both the heart and brain.
In considering that poor diet is now the leading killer globally and mental disorders account for the largest burden of global disability, the fact that diet appears to play a role in mental as well as physical health (as well as increasing the risk of dementia) must be taken very seriously.
Supplements
Yes, proper diet is critical. However, there are a variety of supplemental nutritional needs that are difficult to come by (even with a great diet) that our brains require as we age to help maintain sharp mental acuity and positive cognitive function. Natural supplements can combat certain health, lifestyle, and environmental factors that can increase the risk of cognitive decline and dementia, including:
- Inflammation
- Poor Diet
- Insulin Resistance
- Lack of Exercise
- Poor Sleep
- High Blood Pressure
- Toxins
- Stress
- Social Isolation
Below is a short list of some of the most effective supplements available today that support healthy cognitive function as we age.
CoQ10 (Coenzyme Q10)
This naturally occurring antioxidant that reduces the proliferation of free radicals is produced in the human body for cellular growth and maintenance. Unfortunately, levels of CoQ10 decrease as we age. CoQ10 supports nerve health, the protection of brain tissue from oxidative damage and reduces the action of harmful compounds that can lead to brain disease. In addition, CoQ10 supports healthy cardiovascular function and may reduce the risk for repeat heart attacks and helps combat side effects of cholesterol-lowering statins.
Ginkgo Biloba
This naturally occurring ingredient derived from a tree in Asia can support a healthy inflammation response, supports the production of important brain-building factors, supports recovery from heavy metal/mold exposure, supports healthy blood flow, and supports the brain’s repair from physical trauma.
Phosphatidylserine
This is hard to say but the simple ingredients support a healthy blood sugar response, provide important building factors, and support the brain’s recovery from trauma. The 80+ million Americans living with diabetes or pre-diabetes are at particular risk of cognitive decline given the inability of the body to effectively manage glucose levels.
Coffee Fruit Extract
Derived from the same plant as the coffee bean (although often discarded in favor of the coffee bean!) helps support healthy blood sugar response and increases the brain’s production of key building factors like brain-derived neurotrophic factor (BDNF) that build proteins found in the brain.
Yamada Bee Propolis
Extracted by bees and combined with specific plant proteins to help protect themselves, this supplement supports healthy inflammation response, supports healthy blood sugar levels, supports the production of brain-building factors, supports recovery from exposure to heavy metal and mold exposure, supports normal blood flow, and supports brain repair from trauma.
Turmeric
Many Americans have this tasty spice in their kitchen cabinets, but it is too often left unused! Curcumin, a substance found in Turmeric helps support healthy inflammatory response, provides brain-building compounds, and supports recovery from heavy metal and mold exposure.
Gotu Kola
This herbal extract (from the parsley family) is commonly found in traditional Chinese medicine. This derivative has been used for thousands of years and helps support a healthy inflammatory response, healthy blood flow, and supports brain repair from trauma.
Don’t forget, what you do with your body matters too!
Have you heard that ‘sitting is the new smoking’? When we sit around and let our brains wonder ‘what will be the cause of our demise’, most of us think about heart disease, diabetes, cancer, dementia, old-age, pneumonia, disease, etc. But, according to new data the chair you sit in most is one of the biggest threats to your health. No, this doesn’t mean you should immediately go and throw out your favorite chair, rather it’s time to consider having ‘the talk’ with your favorite chair and let it know you need to get out and stretch your legs more!
Rather than try and come up with our own novel scary statement about how we need to get up from our chairs and be more active, we believe Dr. James Levine, a professor of medicine at the Mayo Clinic has said it best:
“Sitting is more dangerous than smoking, kills more people than HIV, and is more treacherous than parachuting. We are sitting ourselves to death…. the chair is out to kill us.”
—Dr. James Levine, Mayo Clinic
To put it in to perspective—we were not designed to sit. Think about it—we are bipedal for a reason and sitting isn’t the reason. The body is meant to stay in perpetual motion until rest is required. Humans have been on the planet way longer than the chair was invented.
If right about now you are thinking ‘but I exercise, so this can’t apply to me’, unfortunately that doesn’t hold true. Yes, exercise is good for you, and we all need to do more of it; but it doesn’t negate the damage we do to our bodies by sitting for extended periods of time, day after day. Thus, it stands to reason that more exercise is not the answer to sitting too much. Sadly, 10 hours of stillness in a chair (which is not uncommon for people at work) cannot be offset by 1 hour of exercise.
Sitting for long periods of time changes you. It changes your metabolism. It changes the way your body behaves and stores nutrients. In fact, your metabolism can slow down by as much as 90% after only 30 minutes of sitting.
Sitting too long increases the risk of nearly everything that can kill you, including increased rates of:
- Type-2 Diabetes
- cardiovascular disease
- obesity
- disturbed sleep
And increased risk of:
- back and neck pain
- cancer
- deep vein thrombosis
- anxiety and depression
- Alzheimer’s and dementia
- premature death
So, what is the best way to combat ‘sitting too much’. While this is particularly hard for those who work at a desk, it can also be a challenge for many people living with the social isolation that accompanies hearing loss. For starters, get in the habit of standing and/or walking at least once every 20 minutes. With the advent of computers that fit on our wrist, we can now set up simple re minders that get us to ‘stand’. We particularly like smart watches that will not stop reminding you until you stand up!
The goal is to gradually extend our periods of standing and increase the frequency of taking short walks. This is not about engaging in a newfound cross-fit exercise program, but rather increasing the frequency (not the intensity) of physical movement. There are many things we can do every day to increase our standing-to-sitting ratio. When you are at home or work, here are some simple things you can do each day to change your sit ting habit:
- Drink a lot of water (while good for you, this also has the advantage of making you walk to the bathroom more often).
- Talk and walk (when reaching out to a friend or col league on the phone, take the call ‘to-go’ and walk around).
- Pay your bills standing up (instead of sitting at your desk to pay your bills- stand at the counter-height island and pay your bills!).
- Meet up for a coffee and a walk (next time you meet somebody for a coffee why not walk and talk rather than sit down).
- Park further from the entrance to wherever you are going (i.e., take the furthest available spot at the supermarket).
- Take the stairs (now that you drink lots of water, try and use the bathroom furthest away in your house, preferably up or downstairs!).
In addition to the extra movement that you will have from sitting less, a little bit of exercise truly goes a long way. A simple regular exercise regimen can increase your metabolism, help you keep cancer, diabetes, heart disease and obesity at bay, and keep you socially active (i.e., the opposite of social isolation!). If you do not know what pickleball is—it is the fastest growing sport in our country for those over 50 years young. Although we have unofficially nicknamed the game ‘tiny tennis’, it provides BIG benefits by increasing heart rate, burning calories, requiring hand-eye coordination, boosting your balance, and we guarantee you will smile when you play (which is a great workout for your face muscles!).
Always take the opportunity to talk to your hearing healthcare provider and primary care physician about a holistic approach to living your best life.







 Proudly Canadian and Independently Owned and Operated
Proudly Canadian and Independently Owned and Operated 

